Researchers are increasingly using 3D cell cultures to study the skin’s features. Three-dimensional skin models offer the potential to study various diseases and test compounds in vitro. Dr. Florian Groeber-Becker from the Fraunhofer Institute for Silicate Research ISC in Wurzburg has developed a highly sophisticated skin model.
Building the body’s barrier:
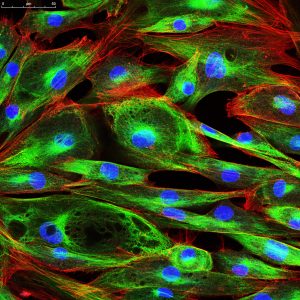
A few cell types constitute the human skin. Fibroblasts (shown here), keratinocytes, and melanocytes are essential cell types.
The evolution of a 3D skin model
One essential application of models in cell culture is for studying wound healing. In 2015, this need led Groeber-Becker and his colleagues to develop a full-thickness skin equivalent along with a device that automatically generates wounds, called ArtCut® (Rossi et al., 2015). “We used dermal fibroblasts in a rat-tail collagen hydrogel without vascularization to model the dermis. On that layer, we seeded human epidermal keratinocytes, and grew them at air-liquid interface to form a multilayered epidermis,” Groeber-Becker explains. “Using this model, it is possible to investigate the effects of drugs and other substances on the healing process. It was a significant first step, but the model has its limitations.” For his subsequent research project, Groeber-Becker made a few changes (Groeber et al., 2016). “The scaffold for our new model is a decellularized piece of porcine jejunum that was vascularized. We call this platform technology “biological vascularized scaffold,” or BioVaSc for short. This piece of matrix is seeded with primary human epidermal keratinocytes (NHEK), dermal fibroblasts (NHDF), and dermal microvascular endothelial cells (HDMEC) at their physiological position,” Groeber-Becker explains. “We cut the piece of the jejunum longitudinally, and place it in a frame. In this way, we receive a flat vascularized skin model after approximately 28 days.” The cells are grown and maintained in a bioreactor at air-liquid-interface. “The media from PromoCell, especially the Keratinocyte Basal Medium 2, supported our experiments tremendously,” he adds. Groeber-Becker’s 3D model overcomes limitations of non-vascularized skin models. Until now, using animal-derived material was the only method available for achieving physiological vascularization in a skin equivalent. After development, the in vitro model showed a dermal and an epidermal layer, with vascularization only in the dermis, which reflects conditions in the human skin. The BioVaSc approach allows researchers to generate other tissue equivalents such as liver (Linke et al., 2007).Applications in biomedical research
A vascularized skin model enables scientists to address additional research areas, including drug development. “We can investigate, for example, the amount of a certain substance that enters blood vessels when it is topically applied to our skin model,” says Groeber-Becker. Researchers can also broaden the applications of the model. “When you add skin cancer cells, you can build your own melanoma model. And, after applying immune cells, you can integrate immunological effects into the skin model. Those are just two examples,” he says. Groeber-Becker expects 3D skin models to move along the path towards increasing complexity in their ability to approximate in vivo conditions. He envisions the possibility of a widespread application of full-thickness skin models. Such a model consists of basement membrane, dermis, and epidermis, and it displays the morphology and functionality of human skin (Ackermann et al., 2010).One major advantage of sophisticated skin models that come close to in vivo conditions is that they minimize the need for experiments on animals. This reduces the suffering of mice, which are used extensively for xenograft experiments in oncology, for example. “Some systemic effects can still be investigated only in animals, but the number of test animals could be reduced dramatically,” Groeber-Becker emphasizes. Good in vitro models could make that possible.

Consultant for PromoCell customers:
Dr. Stéphanie Bonnet is Scientific Application Manager at PromoCell. She advises scientists who want to establish 3D dermatology cell cultures at their institutes.
The transition from 2D to 3D cell culture
Whether for medical or cosmetic applications, many research areas focus on the skin, and the problems are quite similar. “We have many customers who want to establish 3D cultures in their dermatology cell culture. In most cases, the method is well established in two dimensions, but 3D remains a challenge,” Bonnet says. PromoCell offers many products, which means that customers can connect the pieces of puzzle and create their own individual models. But they are not alone, because Bonnet and her colleagues stand by, ready to assist them. “I am a scientist by training, but now I am a consultant, so I’m there whenever our customers need support.” This is how she helps researchers everywhere who are leading the way to scientific progress.Video: How to Generate Standardized Wounds
ArtCut® is the name of a device that automatically generates wounds. In 2015, Dr. Florian Groeber-Becker and a team of researchers developed ArtCut®, along with a full-thickness skin equivalent. To model the dermis, they used dermal fibroblasts in a rat-tail collagen hydrogel. Read the full protocol, and watch the video from the Journal of Visualized Experiments.
Find out more
Related resources
Related pages
REUTER ET AL., (2017): PREPARATION OF A THREE-DIMENSIONAL FULL THICKNESS SKIN EQUIVALENT
In vitro test systems are a promising alternative to animal models. Due to the use of human cells in a three-dimensional arrangement that allows cell-cell or cell-matrix interactions these models may be more predictive for the human situation compared to animal models or two-dimensional cell culture systems.
LANGE ET AL., (2016): INTERACTIONS OF DONOR SOURCES AND MEDIA INFLUENCE THE HISTO-MORPHOLOGICAL QUALITY OF FULL-THICKNESS SKIN MODELS
Human artificial skin models are increasingly employed as non-animal test platforms for research and medical purposes. However, the overall histopathological quality of such models may vary significantly. Therefore, the effects of manufacturing protocols and donor sources on the quality of skin models built-up from fibroblasts and keratinocytes derived from juvenile foreskins is studied.
GROEBER ET AL., (2016): A FIRST VASCULARIZED SKIN EQUIVALENT AS AN ALTERNATIVE TO ANIMAL EXPERIMENTATION
This study demonstrates the generation of a vascularized skin equivalent with a perfused vascular network by combining a biological vascularized scaffold (BioVaSc) based on a decellularized segment of a porcine jejunum and a tailored bioreactor system
