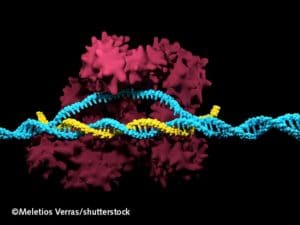
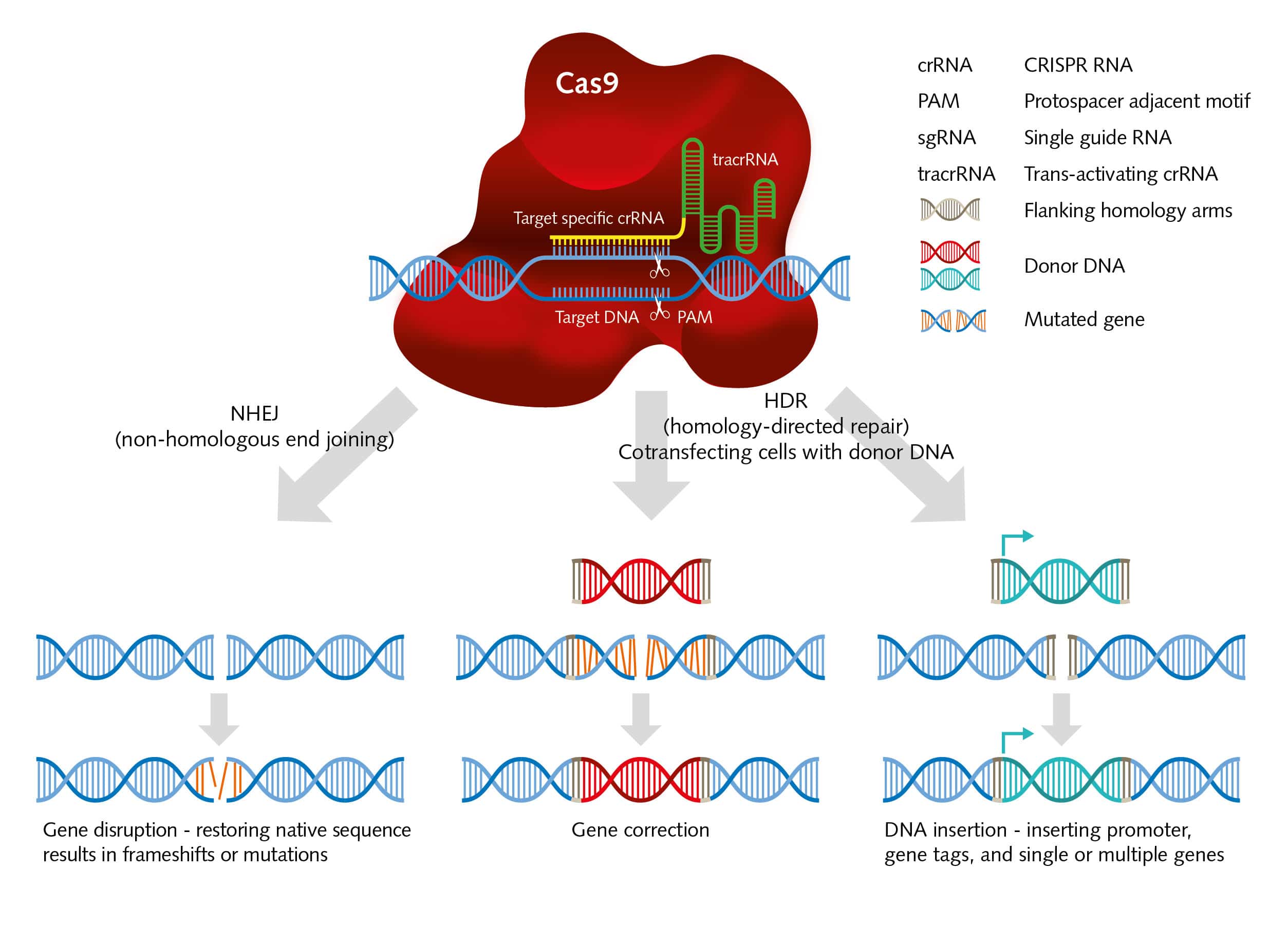
 There are moments in science when everything works out perfectly. When a researcher makes a discovery that ends up revolutionizing an entire field. This doesn’t happen often, but it became reality for a group of researchers around Dr. Emmanuelle Charpentier and Dr. Jennifer Doudna. They co-invented a novel technique for editing genes – the so-called gene scissors (Jinek et al., 2012). The system is built from two components: A chain of nucleotides called Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR), which encodes the guide RNA for recognizing a DNA template, and a protein called CRISPR-associated (Cas) that acts as an endonuclease and uses the guide RNA to site-specifically cut this DNA. This innovative method for editing genes is easy to use and highly precise.
There are moments in science when everything works out perfectly. When a researcher makes a discovery that ends up revolutionizing an entire field. This doesn’t happen often, but it became reality for a group of researchers around Dr. Emmanuelle Charpentier and Dr. Jennifer Doudna. They co-invented a novel technique for editing genes – the so-called gene scissors (Jinek et al., 2012). The system is built from two components: A chain of nucleotides called Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR), which encodes the guide RNA for recognizing a DNA template, and a protein called CRISPR-associated (Cas) that acts as an endonuclease and uses the guide RNA to site-specifically cut this DNA. This innovative method for editing genes is easy to use and highly precise.
After reading the groundbreaking paper of Charpentier and Doudna in Science, hundreds of scientists began employing the new method in their research. As a consequence, the number of papers dealing with CRISPR/Cas9 in the pubmed database quickly rose from 100 in 2012 to 3,000 in 2017.
Treating human immunodeficiency virus using gene scissors

The method fueled many areas in the life sciences such as biomedical research, where it boosted the prospects of human gene therapy in particular. Still, “we have to manage the expectations of the public,” emphasizes Dr. Kathleen Börner, postdoc at Heidelberg University Hospital, who works in the laboratory of Professor Hans-Georg Kräusslich. For her work on CRISPR/Cas9, Börner closely collaborates with another research group in the Department of Infectious Diseases/Virology. This group analyzes virus-host interactions and is led by Professor Dirk Grimm. Börner’s long-term aim is to cure patients of human immunodeficiency virus (HIV) infections using the molecular scissors to excise viral DNA. This is the only way to truly heal patients infected with HIV, because the virus integrates into the genome of CD4+ T cells, after it has used the surface receptor to enter these cells (Paiardini and Müller-Trutwin, 2013). In the long run, untreated HIV infections can cause immunologic complications and mortality, often due to a depletion of T cells. “We want to reverse the process and eliminate the lentivirus before the acquired immunodeficiency syndrome (AIDS) develops,” says Börner.
The researchers recently achieved a first proof-of-principle in cell culture (Kunze et al., 2017). “Now we are planning to move on to in vivo experiments with humanized mice,” says Börner. Such mice have been modified to contain molecular characteristics from humans, in particular components of the immune system, to better mimic conditions in humans (Yong et al., 2018). To eliminate HIV from host cells, the researchers chose an approach where they aim at many targets: “We follow a multiplexed genome editing strategy and add different guide RNAs to our CRISPR/Cas9 cocktail.” By doing so, the researchers inactivate more viral factors and concurrently suppress the emergence of resistant HIV strains, to increase the success of their treatment overall.
Nowadays, Börner turns her attention to the prevention of infection as well. “Researchers have learned a great deal about HIV infection mechanisms. We know of individuals with mutations that render them resistant to HIV infection.“ Such cases of natural HIV resistance occur where the C-C chemokine receptor type 5 (CCR5) is mutated, and therefore nonfunctional (Lopalco, 2010). HIV uses the co-receptor to enter the cells. This offers the following advantage: “Individuals with mutated CCR5 are, to some extent, protected from HIV infection.” There are two sides to the role of CCR5 – its loss of function can be helpful in preventing HIV infection, but studies show an increased risk of other viral infections such as West Nile virus and Influenza virus (Keynan et al., 2011). This is why inactivation of such host factors has to be considered carefully. However, installing immunity against a disease that caused one million deaths globally in 2016, according to the World Health Organization, makes this an option that should at least be considered.
CRISPR/Cas9 in cell culture

Börner and her colleagues achieved their results in cell culture. “There are a few things you should keep in mind when working with primary cells and CRISPR/Cas9. You have to make sure that you introduce or express enough guide RNA and enzymes into or in the cells you want to edit,” says Börner. Researchers have identified different vectors and strategies for transporting those molecules into a cell. These include using physical delivery methods such as electroporation, and non-viral delivery methods such as liposomes, as well as applying viral vectors such as lentiviruses and adenoviruses (Ren and Zhao, 2017, Lino et al., 2018) . Professor Grimm and his group use mainly adeno-associated viruses (AAV) to deliver the gene scissor machinery to the cells (Senís et al., 2014).
Since the use of CRISPR/Cas9 started in 2012, the method has made an unparalleled triumphal march through laboratories worldwide. Börner explains some of the reasons for this. “The system is quite easy to use and compact. We work with only two viral vectors to deliver the entire machinery,” she explains. “You can also multiplex the reaction and target more than one genetic locus. In comparison to other tools for genome editing, such as zinc finger proteins and transcription activator-like effector nucleases (TALENs), the huge advantage of CRISPR/Cas9 is that it uses a nucleotide template for identifying the sequence to be cut. This makes it very easy to use, and it is also quite flexible.” However, there are challenges as well: “With CRISPR/Cas9, there is a certain possibility of off-target cutting events. Particularly when you think about gene therapy, it is extremely important to make sure that only the gene responsible for the disease is cut.”
Gene therapy: state of the art

Despite the challenges, CRISPR/Cas9 has boosted research such as Börner’s that aim to heal diseases. The idea of gene therapy has been around for decades, and when the first trials started in 1990, researchers experienced successes as well as setbacks (Kaufmann et al., 2013). Today, nearly 30 years later, they have built on these experiences and have added sophisticated tools such as CRISPR/Cas9. “We still have to do a lot of groundwork, but I think that we are on our way to truly healing diseases,” says Grimm. In addition to HIV, promising fields for gene therapy include congenital eye diseases, hereditary immune system disorders, and T-cell therapy for cancer, hemophilia B and others (O’Reilly et al., 2014).
Börner is well aware that progress in the field of genome editing relies heavily on public opinion. “It is important to talk about the tools we use and the consequences that our research could have. For people on the street, it is easy to understand why using CRISPR/Cas9 to treat incurable diseases makes sense. However, there are many more applications, so we have to inform people, and initiate a dialogue on the risks and opportunities.” CRISPR/Cas9 is more than a new tool for gene therapy; it is an extremely promising method for basic research as well. It could allow scientists to unravel the mystery of the genetic code and understand the role of particular genes for the physiology of an organism.
Quo vadis CRISPR/Cas9?
The CRISPR/Cas9 system is still under development. Börner calls the progress of the past years a true “joint effort,” as thousands of research groups worldwide are now working with the tool invented by Charpentier and Doudna. “A new application is creating base editor systems, where researchers change only one nucleotide of a triplet to introduce a Stop Codon, for example (Zheng et al., 2018). Another trend Börner is excited about is catalytically inactive CRISPR-associated 9 nuclease (dCas9) that can be used to (in)activate a human gene instead of cutting and disrupting its function (Maeder et al., 2013, Lo and Qi, 2017).
The widespread adoption and easy application have made CRISPR/Cas9 – roughly five years down the road – a game changer. Such an invention translates into prestige and money when it comes to patent registration and commercialization, which is the flipside of the coin regarding the revolutionary discovery of Charpentier and Doudna. Since they published their first paper describing the method of CRISPR/Cas9 and its application in bacteria, there has been an ongoing fight with the research group around Feng Zhang from the Broad Institute in Boston who was first to publish a paper describing the application of the technique in eukaryotes (Ledford, 2017). Despite the fight on patent issues CRISPR/Cas9 remains a revolutionary innovation and a gushing well of new insights.
Five quick facts on CRISPR/Cas9
MEANING: Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) that encode a guide RNA to identify a specific DNA sequence. The CRISPR-associated (Cas) protein acts as an endonuclease
ORIGIN: Bacterial adaptive defense mechanism against viral infections and bacteriophages
HISTORY: First publication on the use of this mechanism as a molecular tool in 2012
SCOPE: CRISPR/Cas holds great potential for gene editing because it cuts specific DNA sequences, it is easy to use and can be adapted quickly to different DNA sequences. It is even possible to multiplex the reaction and target more than one gene sequence at a time.
APPLICATIONS: From basic research to gene therapy for patients with hereditary diseases